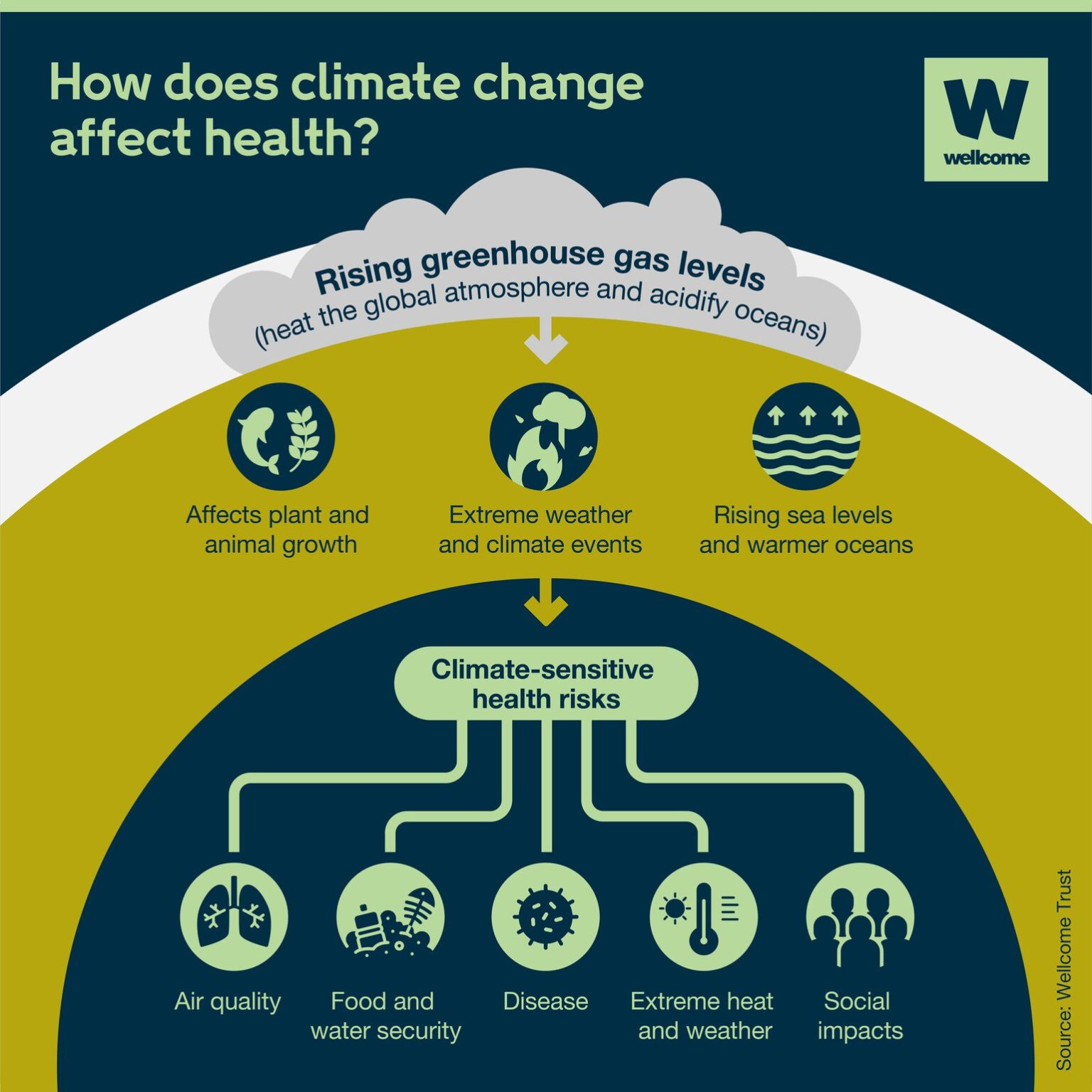
Climate change is a global concern that extends far beyond environmental considerations. It has profound implications for human health and well-being. In this article, there will be exploration of the intricate relationship, between climate and health, focusing on how weather conditions and climatic variables affect public health. With a particular focus on Nigeria, it explores the challenges posed by climate-related diseases such as malaria and meningitis, and how predictive models are helping to mitigate these health risks:
Climate and health: A complex nexus
Human health is intimately linked with the environment, and climate plays a pivotal role in shaping health outcomes. Weather conditions and climatic variables have both direct and indirect impacts on public health. One significant aspect is the seasonality of diseases, where certain illnesses become more prevalent under specific climatic conditions. This phenomenon is often attributed to the rapid breeding and reproduction of disease vectors and microorganisms favoured by particular climates.
The malaria menace
Malaria remains a major public health challenge in Nigeria. According to the World Health Organisation (WHO), Nigeria accounted for a staggering 26.8% of global malaria cases and 31.9% of malaria-related deaths in 2020. The Nigeria Centre for Disease Control (NCDC) reports that a staggering 97% of Nigerians are at risk of malaria, affecting nearly 100 million people annually and causing approximately 300,000 deaths in the country.
Malaria vigilance forecast
Malaria transmission is closely tied to climatic factors, primarily temperature and relative humidity. Based on these factors, Nigeria Meteorological Agency (NiMet) issues a vigilance forecast. When temperatures range between 25°C and 32°C, coupled with relative humidity exceeding 80%, high vigilance is warranted. Moderate vigilance is recommended for temperatures, between 20°C and 25°C with relative humidity between 70% and 80%. Low vigilance is issued when temperatures fall within the 18°C to 20°C range and relative humidity is between 60% and 70%. No vigilance is necessary when temperatures are below 18°C and relative humidity falls below 60%.
Meningitis: A seasonal threat
Nigeria lies within the Meningitis Belt of sub-Saharan Africa, a region known for frequent meningitis outbreaks. This deadly disease poses a significant public health challenge, especially in the northern regions of Nigeria. Meningitis outbreaks are seasonal and strongly influenced by temperature, relative humidity, and atmospheric dust concentration.
Meningitis vigilance forecast
NiMet employs predictive models to determine the likelihood of meningitis outbreaks and their spatial distribution. Vigilance levels are categorised as high, moderate, low, or none, depending on the predicted probability of occurrence. High vigilance is declared when relative humidity is less than 20%, temperature ranges from 25°C to 32°C, and dust concentration is between 500 to 2000 µg/m³. For moderate vigilance, relative humidity falls within 20-40%, temperature is between 20°C and 25°C, and dust concentration ranges from 200 to 500 µg/m³. Low vigilance prevails with relative humidity above 40%, temperatures below 25°C, and dust concentration, between 50 to 200 µg/m³ and no vigilance is needed if there is significant rainfall.
Conclusion
Climate change is reshaping our world, and it’s crucial to understand its impact on human health. In Nigeria, where malaria and meningitis remain significant public health challenges, predictive models are helping authorities prepare and respond to outbreaks. By recognising the intricate relationship, between climate and health, we can take proactive measures to protect vulnerable populations and promote overall well-being.